-
肾移植患者中19%~35%出现了肌肉骨骼疼痛,其中由钙调神经磷酸酶抑制剂(calcineurin inhibitors,CNIs)导致的一种双侧、对称性、难治性疼痛被称为钙调神经磷酸酶抑制剂致疼痛综合征(calcineurin inhibitor-induced pain syndrome,CIPS),最常累及双下肢。CIPS由Bouteiller等首次描述,并于1991年由Lucas等在肾移植患者中首次报道[1],最终由Grotz等在2001年命名为CIPS[2]。近20年来,有关移植后疼痛综合征的报道不断出现,包括CIPS、无血管性坏死(AVN)以及反射性交感神经营养不良综合征(RSDS)等,其中CIPS越来越受到人们的关注。该综合征影响了1%~17%的肾、心脏、肺、肝脏、胰腺或骨髓移植患者[3],且均报道与他克莫司或环孢素有关,移植受者中环孢素致CIPS的发生率为1.5%~14%,而他克莫司致CIPS的发生率为2.2%[4]。为了解肾移植受者中CIPS的临床特征及其治疗方法,本研究对目前已发表的病例报告进行了汇总和统计分析。
HTML
-
通过检索PubMed和Google学术等获得可能相关的外文全文或摘要,检索关键词主要包括:calcineurin inhibitor-induced pain syndrome,post-transplant distal limb syndrome (PTDLS),symmetric bone pain syndrome (SBPS),CIPS in chronic kidney disease (CKD),CIPS in chronic kidney disease stage 5 transplantation (CKD5T)。通过检索中国知网、万方、维普等获取相关的中文全文或摘要,检索关键词:钙调神经磷酸酶抑制剂致疼痛综合征,他克莫司致疼痛综合征,环孢素致疼痛综合征,移植后疼痛综合征,移植后骨疼痛。检索时间段为1991年1月至2020年12月,纳入标准为:肾移植受者、病例报告,排除标准为:非肾移植受者、综述和重复文献。经过筛选和研究入组后,共11篇文章,包括15例病例报告和患者。
-
收集患者的年龄、性别、肾移植类型和原发病,患者发生CIPS的时间、临床表现和实验室检查结果,以及针对CIPS的治疗方法和症状改善时间。
-
采用SPSS22.0进行统计分析。分类变量记录为频数和百分比。正态分布的测量值表示为(
$\bar x $ ±s)以及范围,非正态分布的表示为中位数和四分位间距(IQR)。
1.1. 研究对象
1.2. 观察指标
1.3. 统计方法
-
对所纳入的11篇文章(均为外文文章)中的15例肾移植受者进行了定性和定量分析。表1总结了肾移植受者中CIPS的研究[5-15]。诊断时患者的平均年龄为(44.6±8.31)岁(范围为23~59岁)。在这些患者中,有8名(53.3%)男性,7名(46.7%)女性。肾移植的类型包括:尸体肾移植(n=10,66.7%),活体供体(n=3,20%)和数据缺乏(n=2,13.3%)。导致肾脏移植的原发病包括:IgA肾病(n=3,20%),肾小球肾炎(n=1,6.7%),高血压肾病(n=2,13.3%),自身免疫性疾病(类风湿关节炎、系统性红斑狼疮,n=3,20%),镇痛性肾病(n=1,6.7%),左侧肾脏发育不全(n=1,6.7%),伯杰病(n=1,6.7%),病因不明的终末期肾脏疾病(ESRD)(n=2,13.3%)和数据缺乏(n=1,6.7%)。
病例 年龄 性别 肾移植类型 原发病 参考文献 1 41 男 尸肾移植 不明原因的慢性肾功能衰竭 [5] 2 59 女 第二次活体肾脏移植 病因不明的ESRD [6] 3 44 男 左肾发育不全致终末期肾病的肾移植 左肾发育不全 [7] 4 53 女 原发性ABO不相容的活体肾脏移植 控制良好的类风湿性关节炎和慢性肾脏疾病 [8] 5 37 男 活体肾脏移植 伯杰病 [9] 6 48 女 尸肾移植 镇痛性肾病 [10] 7 49 男 尸肾移植 IgA肾病 [10] 8 50 男 尸肾移植 IgA肾病 [10] 9 40 女 尸肾移植 系统性红斑狼疮 [10] 10 50 女 尸肾移植 未提及 [11] 11 49 男 尸肾移植 高血压肾病 [12] 12 42 男 尸肾移植 动脉高血压 [12] 13 23 女 从一名41岁的头部外伤捐赠者那里接受了肾脏同种异体移植 狼疮性肾炎 [13] 14 43 女 第二次尸肾移植 肾小球肾炎 [14] 15 41 男 第二次尸肾移植 IgA肾病和高血压 [15] -
受累的关节表现包括: 双侧膝盖疼痛(n = 4, 26.7%), 双足对称性疼痛(n = 3, 20%), 双侧膝盖和双足疼痛(n = 2, 13.3%), 双足和脚踝疼痛(n = 1, 6.7%), 双侧膝盖和脚踝疼痛(n = 1, 6.7%), 双侧腕、肘、手和膝盖疼痛(n = 1, 6.7%), 双侧手、膝盖、脚踝和双足疼痛(n = 1, 6.7%), 双侧手、肘、膝盖、脚踝和双足疼痛(n = 1, 6.7%), 后背疼痛(n = 1, 6.7%)。肾移植后CIPS出现的平均时间为(2.42±3.07)个月(1例描述为肾移植后不久, 具体时间不详), 中位数为1.22个月, IQR为1~2个月。具体详见表 2。
病例 症状表现 累及关节 症状出现时间 1 双足对称性的严重疼痛 双足 过去的9年 (发生在肾移植后不久) 2 双侧踝关节和膝盖疼痛,双侧下肢左下踝外侧踝乏力 膝盖,脚踝 第2次肾移植后6周 3 首先是左脚疼痛,然后是双脚(在脚趾两侧)和膝盖(在两个膝盖的外侧)进行性疼痛,患处伴有水肿 膝盖,双足 移植后2个月 4 高热,疲劳和关节疼痛 手肘,手腕,膝盖 移植后14 d 5 双脚突发严重的对称性疼痛,行走受限 双足 肾移植后1年 6 突发严重的双侧膝关节疼痛 膝盖 移植后第1个月 7 突发严重的双侧膝关节疼痛 膝盖 移植后第1个月 8 突发严重的双侧膝关节疼痛 膝盖 移植后第1个月 9 突发严重的双侧膝关节疼痛,双足严重的骨痛 膝盖,双足 移植后第1个月 10 膝部进行性双侧对称性疼痛且行走困难 膝盖 移植后2个月 11 运动时多个关节剧烈疼痛,并在移植后2个月使用拐杖走路 双手,膝盖,脚踝和双足 移植后1个月 12 双足疼痛,无法行走 双足 移植后6个月 13 从胸腔到腰骶的严重后背钝痛,疼痛评分为10/10。背部伸展使疼痛加重,背部弯曲和躺下缓解。坐位时,尾骨区疼痛加重;背部中线以外无疼痛辐射 后背 移植后43 d 14 双足和脚踝进行性疼痛 双足和脚踝 术后1个月 15 双侧足部疼痛和轻微的脚踝疼痛,最后延伸至膝盖;4个月后,疼痛变得难以忍受,手和肘部出现轻微疼痛 双足,脚踝,膝盖,手和肘部 肾移植后73 d -
CNIs水平的影响在此研究中是无法估计的, 原因在于缺少实际治疗水平(谷浓度范围)的数据。CIPS发生时, CNIs水平升高或正常。7名(46.7%)患者使用环孢素作为初始免疫抑制药物, 其中6名(40%)测量了环孢素水平, 环孢素的平均全血谷浓度为(194.5±92.9) ng/ml(范围为38~278 ng/ml)。其中3名患者的环孢素谷浓度较高, 平均谷浓度为(268±12.5)ng/ml(范围为254~278 ng/ml)。8名(53.3%)患者使用他克莫司作为初始免疫抑制药物, 其中6名(40%)测量了他克莫司水平, 其平均全血谷浓度为(21.6±9.3) ng/ml(范围为5~28.2 ng/ml)。3名(20%)患者的碱性磷酸酶水平升高, 1名(6.7%)患者的碱性磷酸酶水平正常, 而11名(73.3%)患者的数据缺乏。4名(26.7%)患者的甲状旁腺激素(PTH)水平增加, 平均水平为(260±383)ng/L(范围为26~833 ng/L), 4名(26.7%)患者的PTH水平正常, 7名(46.7%)患者的数据缺乏。3名(20%)患者出现了高钙血症, 1名(6.7%)患者的血清钙水平正常, 11名(73.3%)患者的数据缺乏。2名(13.3%)患者出现低磷血症, 1名(6.7%)患者出现高磷血症, 1名(6.7%)患者血磷水平正常, 11名(73.3%)患者的数据缺乏。1名患者(6.7%)的C反应蛋白升高, 8名患者(53.3%)的C反应蛋白正常, 6名(40%)患者的数据缺乏。2名(13.3%)患者类风湿因子水平正常, 13名(86.7%)患者的数据缺乏。4名(26.7%)患者的尿酸水平正常, 11名(73.3%)患者的数据缺乏。
-
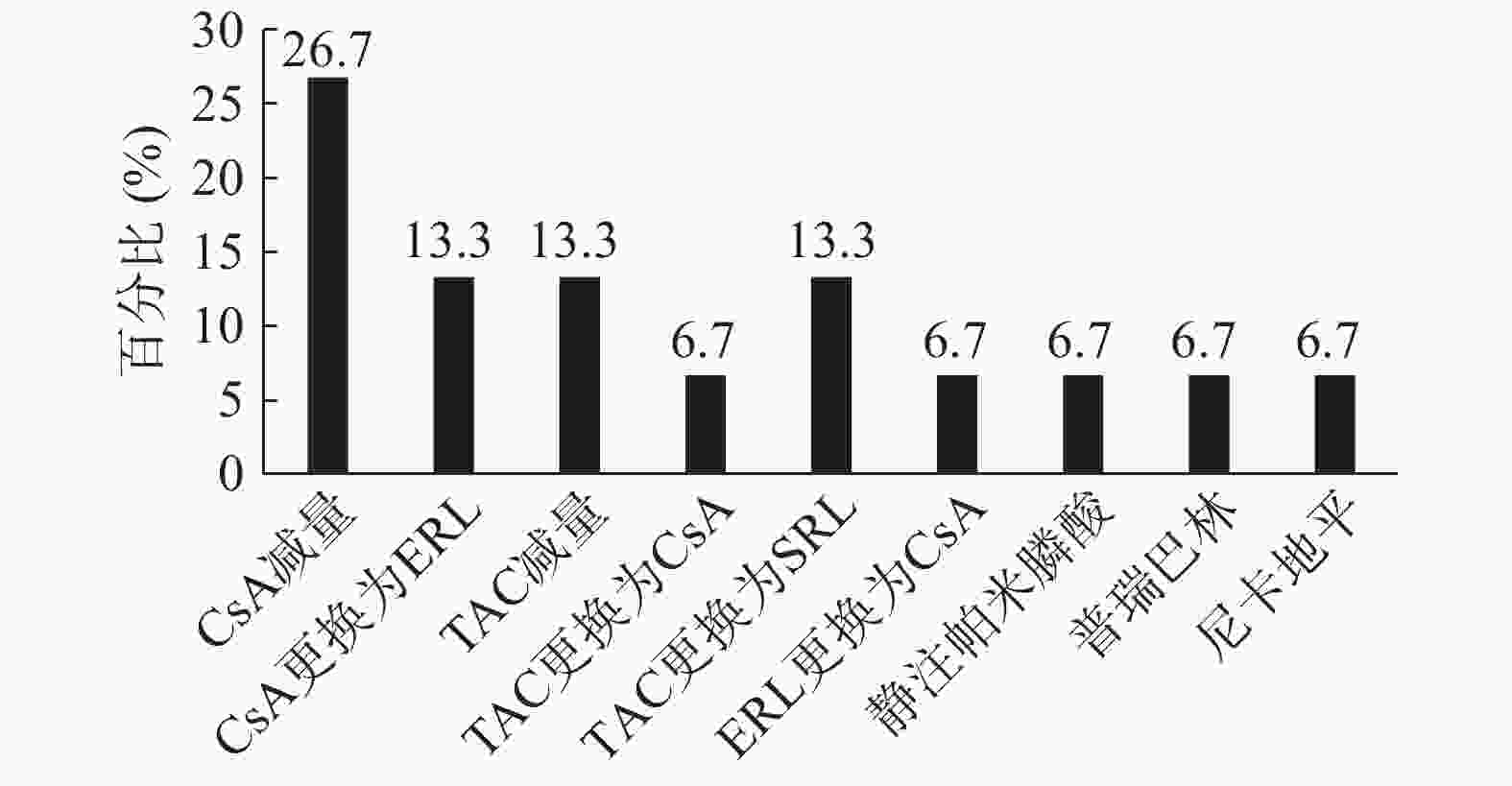
在本研究纳入的15名患者中, 4名(26.7%)患者调整了环孢素剂量, 治疗后3个月症状缓解。1名(6.7%)患者将环孢素更换为依维莫司, 出院后两周和随访4个月后, 疼痛有所改善, 后给予降钙素治疗4周后无临床获益。1名(6.7%)患者开始使用氨氯地平并不能改善其症状, 但将小剂量环孢素更换为依维莫司后, 疼痛得到明显改善。6个月后, MRI显示骨髓水肿消失, 关节周围轻度积液缓解。2名(13.3%)患者在他克莫司减量后症状改善。1名(6.7%)患者在停用他克莫司并更换为CsA1周内其症状消失, 且血清肌酐水平正常, 肾移植术后无急性排斥反应和疼痛。2名患者(13.3%)将他克莫司更换为西罗莫司后症状均改善, 但其中1例在几周后由于华法林引起的脑出血而死亡。将依维莫司更换为小剂量环孢素后2个月, 1名(6.7%)患者的症状改善, 并且未采用任何特殊治疗, 发病后7个月其疼痛症状消失。1名(6.7%)患者在开始静脉注射帕米膦酸后其活动能力有所改善。1名(6.7%)患者在合用克霉唑2 d后出现背部疼痛, 考虑克霉唑导致他克莫司水平升高, 故停用克霉唑, 并给予硝苯地平治疗, 患者背部疼痛无缓解, 但在普瑞巴林首次给药后30 min内患者疼痛评分明显降低, 并在发病后3周疼痛症状消失。1名(6.7%)患者将他克莫司更换为依维莫司后疼痛未缓解, 给予曲马多、氨酚氢可酮、芬太尼、度洛西汀、西那卡塞和双膦酸盐后患者疼痛亦无明显缓解, 但在将硝苯地平更换为尼卡地平后患者疼痛缓解, 最终在移植后9个月症状完全缓解。13名患者的症状好转时间平均为(4.43±3.31)个月, 另外2名患者未描述。CIPS有效治疗方式的分布见图 1。
2.1. 患者特征
2.2. 关节受累的解剖区域
2.3. 实验室指标
2.4. 治疗与结局
-
在本研究中, 肾移植术后出现CIPS的患者无明显性别差异且为中青年人群, 其肾移植类型多为尸体肾移植, 原发病主要为IgA肾病、自身免疫性疾病和高血压。既往研究报道CIPS主要累及下肢, 本研究显示可出现CIPS症状的部位众多, 涉及双侧手、肘、腕、膝盖、脚踝、双足以及后背。CIPS多表现为神经性症状, 如异常性疼痛和电击样疼痛, 也有相关瘙痒的报道。没有营养性皮肤变化或血管舒缩不稳的迹象。体格检查通常是正常的。
本研究中CIPS出现的时间范围为肾移植后14 d至1年, 经治疗后缓解期最短为20 d, 最长可达1年。实验室检查提示发生CIPS时CNIs的谷浓度升高或正常, 部分患者的碱性磷酸酶、甲状旁腺激素、血钙、C反应蛋白水平升高, 血磷水平异常, 而类风湿因子、尿酸水平正常。CIPS已被证实可能发生在肝、肾移植以及干细胞移植中。CNIs阻断可下调背景电流的脊髓钾离子通道, 进而通过影响动作电位传播的速度来增强兴奋性信号传导[16]。Grotz等提出了这样的假说, 即CNIs引起的血管紊乱导致骨髓血管通透性增加并伴有骨髓水肿, 后期报道的一些CIPS患者受累关节中示踪剂摄入增加和轻度骨髓水肿亦证实了这一假说。他克莫司可通过增加潜在的N-甲基-D-天冬氨酸受体(NMDAR)活性导致不受限制的伤害性输入, 并且其磷酸化状态由蛋白激酶和蛋白磷酸酶活性之间的平衡动态控制。酪蛋白激酶II的激活可增加NMDARs的磷酸化和活性, 而钙调磷酸酶可以负反馈调节大脑中NMDARs的磷酸化及其功能。尽管CNIs导致脊髓NMDAR活性增加的机制尚不完全清楚, 但在CIPS中, CNIs可能通过抑制钙调磷酸酶的活性, 使脊髓背角中NMDARs的磷酸化/去磷酸化周期转变为以磷酸化状态为主[17]。初级感觉神经元和脊髓背角神经元的中央末端之间的第一感觉突触在感觉信息的传递和转换中起着重要作用。谷氨酸是一种重要的兴奋性神经递质, 而NMDARs在与背角疼痛传导相关的脊髓突触可塑性中起着关键作用[18]。
针对CIPS的药物治疗中, 阿片类镇痛药如吗啡、芬太尼、羟考酮等通常对CIPS无效。非甾体类抗炎药可以缓解症状, 但会对肾功能产生不利影响。据报道, 核心减压可迅速改善短暂性骨髓水肿的症状, 但如果保守处理, CIPS和短暂性骨髓水肿通常会在2~4个月内改善。氯膦酸盐和降钙素的使用似乎可以通过抑制骨溶解来减轻疼痛。CNIs减量或停用也可以缓解疼痛症状。在许多情况下, CNIs交换(如从他克莫司更换为环孢素或从环孢素更换为他克莫司)是有效的。下肢疼痛时建议将腿抬高。使用不抑制细胞色素P450的钙通道拮抗剂似乎也能有效地降低骨内高压。前列环素类似物伊洛前列素可能至少在重症患者中是一种安全的治疗选择。在Tillmann等进行的一项原始研究中, 采用标准方案静注伊洛前列素治疗10名患者, 通过评分从1~10的视觉类似量表测量, 结果表明伊洛前列素可促进疼痛的缓解: 治疗前(5.6±1.5), 治疗后(2.1±1.3), P = 0.0004[19]。Taşoğlu等的病例报告中首次描述了通常能有效用于神经性疼痛的γ-氨基丁酸(GABA)类似物, 如加巴喷丁或普瑞巴林。作者介绍了一名48岁接受了肝移植手术的男性患者, 该患者出现了双脚剧烈疼痛, 且疼痛程度逐渐增加, 有时甚至累及到膝盖。而给予普瑞巴林150 mg, 每天2次, 显著减轻了他的疼痛[20]。尽管已描述了在使用双膦酸盐(30 mg)后, CIPS症状得到改善, 但目前对其有效性仍存在争议。本研究中76.9%(10/13)的肾移植受者通过将CNIs减量或将CNIs更换为同类药物中的另一种药物, 使CIPS症状得到了缓解, 其他缓解症状的方法还包括静脉注射帕米膦酸、使用普瑞巴林以及尼卡地平。而使用阿片类镇痛药、双磷酸盐、降钙素、氨氯地平或硝苯地平未能明显改善症状。
CIPS是移植受者中发生的一种难治性疼痛综合征, 受累部位广泛, 病程长短不一, 其发病机制仍有待进一步研究。CIPS的最有效治疗方法是减少CNIs的剂量和更换免疫抑制剂, 其他治疗方式包括GABA类似物、帕米膦酸钠静脉注射、钙通道阻滞剂和保守疗法等。









 DownLoad:
DownLoad: