-
结直肠癌(CRC)是最常见的消化道恶性肿瘤,在中国的发病率仅次于肺癌,且呈现逐年升高的趋势[1]。结直肠癌的发病机制具有多因素、多阶段、多基因突变等特点[2,3]。结直肠癌早期发现的概率低,多数患者出现明显症状后才被确诊,此时手术通常已无法完全控制肿瘤进展,需化疗控制病情[4]。结直肠癌患者最常用的化疗药物为奥沙利铂和五氟尿嘧啶(5-FU),分别是DNA合成抑制剂和胸苷酸合成酶抑制剂,影响细胞DNA复制和转录,最终导致细胞死亡[5-7]。近年来,复发/难治性结直肠癌患者逐渐升高,对多数化疗药无应答,其5年生存率低于10%[8-9]。结直肠癌患者耐药情况越来越严重,解决耐药问题的首要条件为阐明结直肠癌患者化疗耐药的机制。
随着人们对肠道微生物研究的深入,已明确表明其与多种肠道疾病相关,其中具核梭杆菌(Fn)与结直肠癌发生发展的关系研究最透彻[10-13]。在口腔、胃肠道、呼吸道等环境内均明确发现Fn,其是一种专性厌氧性、G−菌,可黏附、侵入细胞,获得适合生存的环境[14-16]。Fn可以产生毒力因子、提升白介素17(IL-17)和肿瘤坏死因子(TNF)等促炎因子水平、抑制自然杀伤细胞的细胞毒活性、招募肿瘤浸润性骨髓细胞等,促进肿瘤发生发展和耐药机制的产生[11-13, 17-19]。例如,Fn促进了CRC的进展,并使奥沙利铂和5-FU化疗耐药[20],因此,解决Fn高富集后促进CRC进展并产生化疗耐药的问题,有望提升结直肠癌患者化疗的有效率。
本研究首先在类器官层面验证Fn促结直肠癌增殖作用,其次比较考察前期筛选获得的抗Fn化合物在Fn与结肠癌HCT116细胞共孵育条件下对其体外抗癌活性的影响,最后优选高活性化合物开展其对Fn灌胃干预下裸鼠结肠癌HCT116移植瘤抗癌药效评价,从而为新型抗结直肠癌药物研发提供先导化合物。
-
本研究所用活性化合物购自上海陶术生物科技有限公司;布氏肉汤、脑心浸出液(BHI)肉汤购自美国BD公司;结直肠癌类器官基础培养基、培养基补充液B、培养基补充液C、类器官培养型基质胶、肿瘤组织消化液和红细胞裂解液购自伯桢生物科技公司;直肠癌组织取自海军军医大学第一附属医院肛肠科;DMEM培养基、CCK-8检测试剂盒、胎牛血清购自上海翌圣生物科技股份有限公司;人结直肠癌细胞HCT116购自上海中国科学院细胞中心;具核梭杆菌(ATCC 23726)购自美国模式菌种收集中心;裸鼠购自上海吉辉实验动物饲养有限公司。xCELLigence RTCA DP实时无标记细胞分析仪(安捷伦科技有限公司)
-
①实验前准备:首先,配置完全培养基(结直肠癌类器官基础培养基∶培养基补充B∶培养基补充C=976∶20∶4),其次,将-20°C保存的类器官基质胶放置于4 °C融化(室温下不超过30 s),最后,将肿瘤组织消化液置于37 °C的水浴锅内预热;②组织收集与处理:直肠癌组织用类器官基础培养基清洗2遍,置于盛有PBS的无菌培养皿中,无菌剪刀剪碎组织至直径小于1 mm,然后用适量的肿瘤组织消化液重悬,并转移至离心管内,于37 ℃、100 r/min的恒温振荡培养箱中消化30 min,在消化完成的组织悬液中加入胎牛血清(FBS)至终浓度达1%~5%,减缓消化作用,同时轻轻吹打5~10次;③筛选细胞:用100 μm细胞过滤器过滤组织悬液,将穿过的滤液转移至离心管中,450 r/min离心3 min,吸去上清液;④细胞收集:用类器官基础培养基清洗细胞2次,加入红细胞裂解液裂解1 min,300 r/min离心3 min,吸去上清液;⑤3D培养板细胞接种:按每孔2×103个细胞用20 μl基质胶于冰浴条件下混匀,然后用移液器将基质胶和细胞的混合液移至细胞培养24孔板底部中央位置,于37 ℃、5% CO2细胞培养箱中孵育15 min;⑥加液培养:待培养24孔板基质胶凝固至不再流动后,沿孔壁缓缓加入完全培养基,于37 ℃、5% CO2培养箱中培养;⑦加Fn菌液:培养72 h后,观察类器官成型且稳定,采用完全培养基重悬Fn使其浓度分别为1×108 CFU/ml和1×104 CFU/ml,加入24孔板中,同时在不同孔中加入同体积PBS;⑧观察:每天在同一视野、同一放大倍数下分别对PBS、浓度为1×104 CFU/ml和1 × 108 CFU/ml的Fn作用下的直肠癌类器官进行拍照记录,观察类器官生长变化,共4 d。
-
①细胞培养:用8 ml含10%胎牛血清和1%双抗的DMEM培养基培养HCT116细胞。待细胞生长至 90% 左右时,弃上清液,加入2 ml PBS清洗,2 ml胰酶消化1.0 min,加入3 ml含10%胎牛血清和1%双抗的DMEM培养基吹打均匀,1 000 r/min离心5 min后,弃去上清液,加入4 ml含10%胎牛血清和1%双抗的DMEM培养基再次吹打均匀,取10 μl细胞悬液稀释10倍至100 μl,置于细胞计数板上计数;②细胞铺板:将HCT116细胞按照浓度为每孔7 × 103个/ml加100 μl于96孔板中,37 ℃、5% CO2细胞培养箱中孵育12 h;③受试药物与细胞或与细胞和Fn共孵育:吸出培养基,每孔加入100 μl不同浓度的受试化合物,将生长良好的Fn培养液用4 000 r/min离心10 min,弃上清液,加入无胎牛血清、无双抗的DMEM培养基混匀,比浊仪将菌的浓度调至0.5麦氏浊度[(1~2)×108 CFU/ml]制得Fn菌液,然后再加入100 μl感染系数(MOI)为1 000:1的上述Fn菌液或新鲜无胎牛血清和双抗的DMEM培养基,于37 ℃、5%CO2细胞培养箱中培养72 h;④测定IC50:吸出培养基,加入100 μl浓度为10%的CCK-8溶液,35 ℃孵育0.5 h,在450 nm波长的条件下读取A值;用GraphPad Prism 7软件拟合出受试药物对HCT116细胞或与Fn共孵育HCT116细胞的IC50值。
-
①HCT116细胞培养和Fn菌液准备同“2.2”项;②按实时无标记细胞分析仪的规范操作程序完成名称、目的、分组、时长等输入;③以50 μl含5%胎牛血清、无双抗DMEM培养基进行基线矫正;④每孔加入7×103个/ml 的HCT116细胞,在室温下放置 30 min后,放置于测试台中;⑤ 18 h后暂停设备,吸出培养基,加入含5%胎牛血清、无双抗DMEM培养基的Fn菌液100 μl,使得MOI=1 000∶1,加入浓度在最小抑菌浓度(MIC)上下的受试化合物100 μl,放入测试台中继续培养72 h,实时观察记录HCT116细胞数量变化。
-
①裸鼠在动物房无操作下饲养5 d,然后在裸鼠饮用水中加入链霉素和克林霉素使其浓度分别为5 g/L和0.1 g/L,继续饲养7 d以清理裸鼠肠道微生物,减少其他微生物对实验结果的影响;②以皮下注射方式,接种浓度为1.0×107个/ml的人源HCT116细胞;③待皮下肿瘤大小长至50 mm3时,将浓度为1×108 CFU/ml(BHI溶解)的Fn菌液灌胃,每2 d给予1次,500 μl/只,共4次;④将荷瘤裸鼠随机分为4组,对照组和PD-1组每组5只,甲氨蝶呤组和联合用药组每组3只。对照组:每3 d给予Fn灌胃1次;PD-1组:除每3 dFn灌胃1次外,另外给予PD-1腹腔注射100 μl,首周3次,次周2次,每次给药剂量为5 mg/kg;受试药物组:除给予每3 d予Fn灌胃1次外,再给予甲氨蝶呤灌胃500 μl,给药剂量为0.5 mg/kg,每天给药1次;联合用药组:采用同样的给药频率和给药剂量,同时给予甲氨蝶呤和PD-1;⑤裸鼠体重和肿瘤体积监测:每天监测荷瘤裸鼠体重和皮下肿瘤体积变化,观测15 d后断颈处死裸鼠。肿瘤体积计算公式为V=1/2×a×b2;式中a为肿瘤长径,b为肿瘤短径b。抑瘤率(%)=(对照组平均体积-实验组平均体积)/对照组平均体积× 100%。
-
实验处理及统计图表的绘制利用GraphPad Prism软件完成。符合正态分布计量资料用(
$ \bar{x}\pm \mathrm{s} $ )描述,进行方差分析或t检验,计数资料采用$ {\chi ^2} $ 检验。P<0.05为有统计学差异。 -
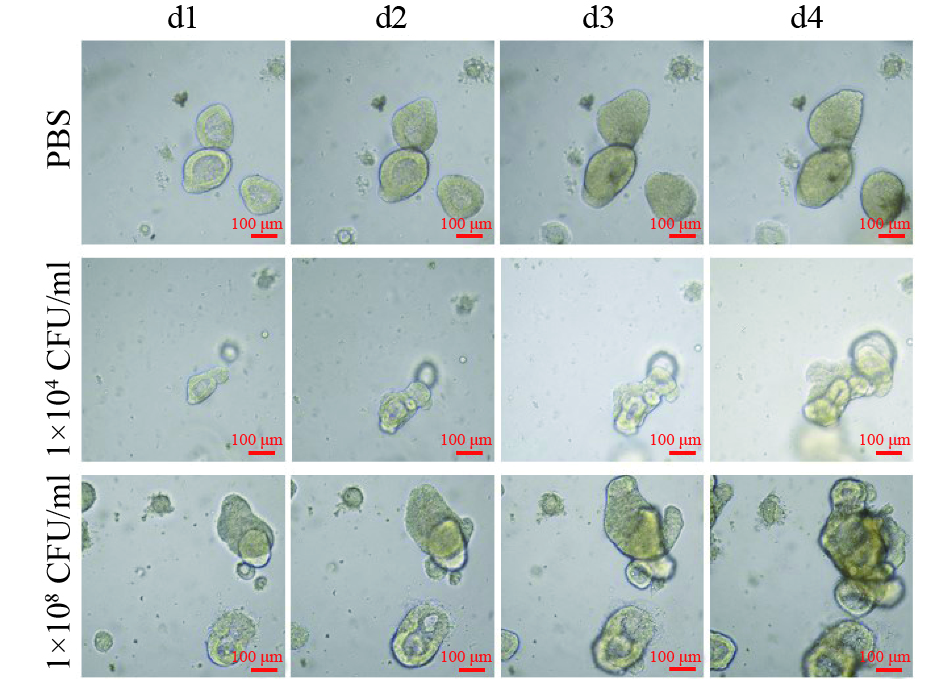
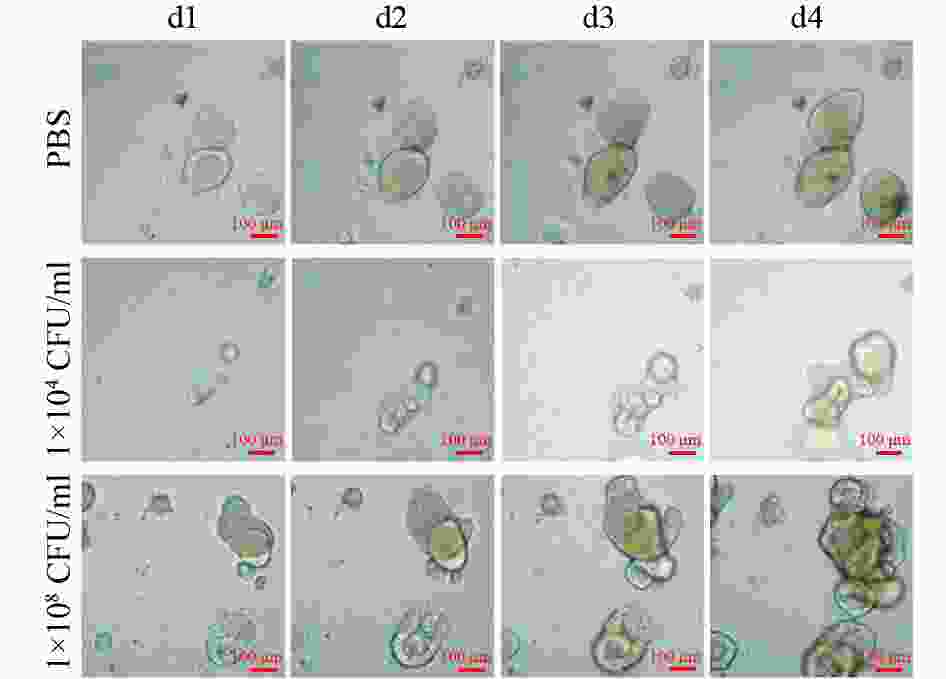
连续4 d对PBS和不同浓度Fn干预下的固定位置直肠癌类器官生长情况的拍照观察结果显示,PBS阴性对照组的直肠癌类器官随时间呈缓慢生长;但是,1×104 CFU/ml浓度的Fn干预下的直肠癌类器官随时间呈急速生长,且呈浓度依赖(图1)。
-
用CCK-8法分别比较测定了前期筛选获得的9个MIC达2.0~32 μg/ml的抗Fn活性化合物对人结直肠癌HCT116细胞及在最优MOI条件下与Fn共孵育的人结直肠癌HCT116细胞的体外IC50,结果显示,9个受试化合物均能显著提升Fn与结肠癌细胞共孵育条件下的体外抗肿瘤活性,其中,甲氨蝶呤提升幅度最大,达143倍(表1)。
名称 MIC
(μg/ml)HCT116
(IC50,μmol/L)HCT116 + Fn
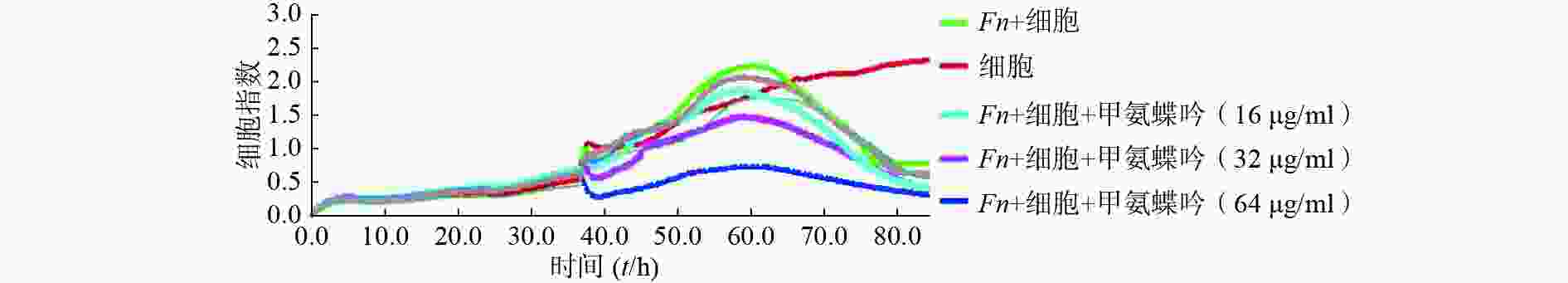
(IC50,μmol/L)新鱼腥草素钠 32 0.48 0.12 对甲氧基苯甲醛 32 4.22 1.77 PA-824 32 9.62 5.62 甲氨蝶呤 32 4.30 0.03 吲哚-3-甲酸 16 8.86 2.72 己烯雌酚 32 23.10 9.35 2'-脱氧胞嘧啶核苷 8 0.78 0.07 5-硝基-8-羟基喹啉 2 22.85 3.93 特地唑胺 2 4.29 1.42 通过实时无标记肿瘤细胞分析技术检测了优选抗Fn活性化合物甲氨蝶呤在Fn与HCT116细胞共孵育条件下对肿瘤细胞生长的影响,实时检测结果显示,甲氨蝶呤也能显著抑制Fn的促肿瘤细胞生长作用,且呈浓度依赖性(图2)。
综上所述,优选甲氨蝶呤开展后续Fn灌胃干预下裸鼠人结肠癌HCT116移植瘤的体内抗癌药效评价。
-
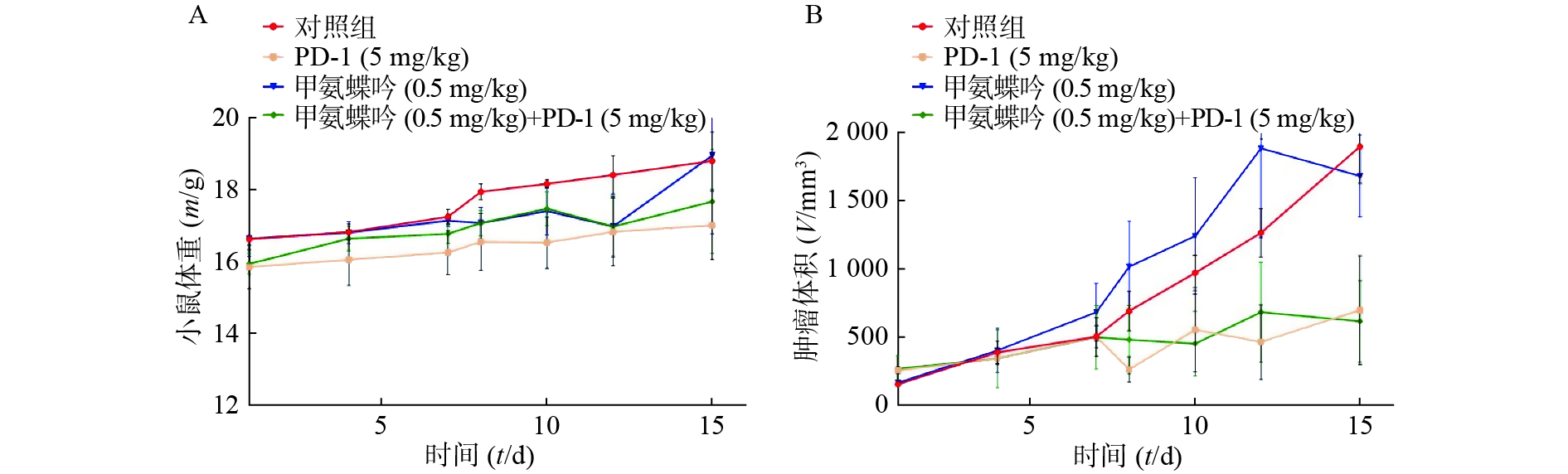
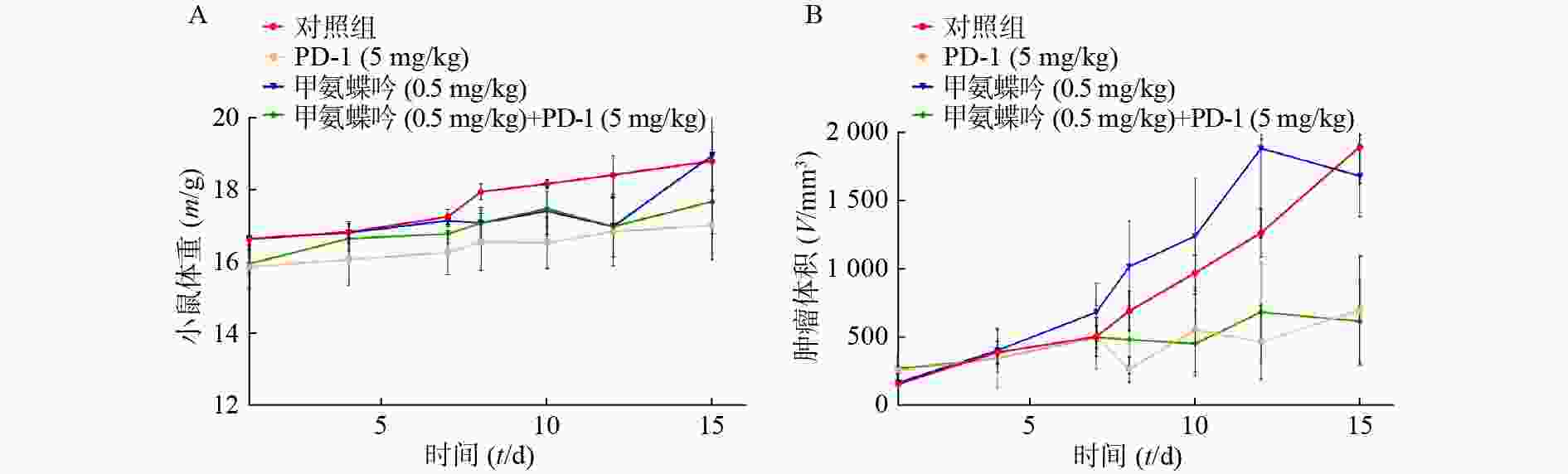
在Fn灌胃干预下,抗Fn优选化合物甲氨蝶呤(0.5 mg/kg)以及PD-1(5.0 mg/kg)单独用药的抑瘤率分别为11.39%、53.95%;当甲氨蝶呤(0.5 mg/kg)与PD-1(5.0 mg/kg)联用后,其抑瘤率可显著提升至67.46%(表2和图3B)。给药组荷瘤裸鼠的体重无显著变化,与对照组相似(图3A)。
组别 PD-1 甲氨蝶呤 单独用药 53.95% 11.39% 联合PD-1 − 67.46% $ {\chi ^2} $ − 65.82 P − <0.01 -
本文研究表明:首先,Fn(1 × 104 CFU/ml)可显著促进直肠癌类器官增殖,且呈浓度依赖(图1);其次,9个抗Fn活性化合物(MIC= 2.0~32 μg/ml)均能显著提升与Fn共孵育结肠癌HCT116细胞的体外抗肿瘤活性,其中,甲氨蝶呤提升抗癌活性幅度最大,达143倍(表1),同时,实时无标记肿瘤细胞生长分析实验显示,甲氨蝶呤也能显著抑制Fn促结肠癌HCT116细胞生长作用,且呈浓度依赖特性(图2);最后,抗Fn优选活性化合物甲氨蝶呤(0.5 mg/kg)与PD-1(5.0 mg/kg)联用,对Fn灌胃干预下裸鼠人结肠癌HCT116移植瘤具有显著的抑制活性,其抑瘤率达67.46%,分别优于相同给药剂量的甲氨蝶呤和PD-1单独用药的抑瘤活性(表2和图3B),且对荷瘤裸鼠的体重无显著影响(图3A)。
总之,本研究可为后续抗Fn类抗结直肠癌药物结构衍生提供先导化合物,并有望拓展甲氨蝶呤的新适应证。同时,本文研究仍有部分缺陷,如体内实验没有设置无Fn灌胃干预组,观察无Fn干预情况下裸鼠移植瘤的肿瘤增殖情况,因此,这也为后续深入结构优化所得高抗Fn活性化合物的体内抗结直肠癌活性研究提供改进策略。
Screening of small molecule inhibitors against Fusobacteriumnucleatum and study of their anti-colorectal activity
doi: 10.12206/j.issn.2097-2024.202405009
- Received Date: 2024-05-08
- Rev Recd Date: 2024-05-21
-
Key words:
- Fusobacterium nucleatum /
- phenotypic screening /
- anti-crc /
- organoids /
- methotrexate
Abstract:
| Citation: | BAI Xuexin, CHEN Yuping, SHENG Chunquan, WU Shanchao. Screening of small molecule inhibitors against Fusobacteriumnucleatum and study of their anti-colorectal activity[J]. Journal of Pharmaceutical Practice and Service. doi: 10.12206/j.issn.2097-2024.202405009 |









 DownLoad:
DownLoad: